Orchiectomy
Conveniently located to serve Seattle and Bellevue
Jump To
Bilateral orchiectomy ultimately leads to decrease in testosterone and loss of sperm production. Circulating testosterone should be minimal made from the adrenal glands. If considering the possibility of children in the future consideration to sperm banking should be done prior to the procedure.
Testicular Anatomy
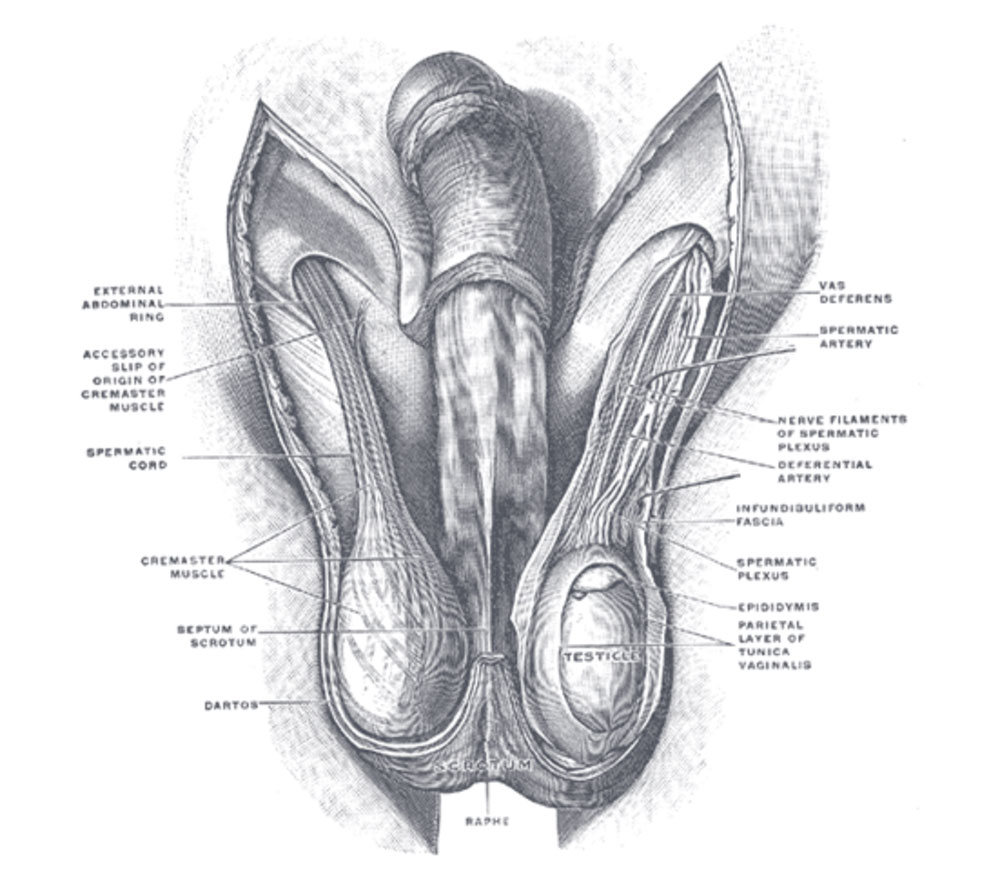
Testicle or male gonads are oval shaped reproductive structures that lie in the scrotum. Their primary function being the production of 1. testosterone and 2. sperm. The scrotum is a sac that is composed of muscle and skin that can contract and alter the temperature within it to maintain optimal conditions for the testicles to function. The testicles can produce about 6 mg of testosterone per day.
Therefore after bilateral orchiectomy there is a significant decrease in testosterone levels, which results in less demand for estrogen supplementation. When starting the surgical transition phase, orchiectomy may be an early option for some.
Reviews
Dr. Parikh and his team were an absolute pleasure to work with. Everyone I met with on the day of surgery was friendly and thorough in their support. He provided great follow-up care and continued to check in with me after surgery. I would definitely recommend Dr. Parikh to anyone who is looking into their options for an orchiectomy.
D.P.
Orchiectomy Procedure
The procedure is relatively straightforward. It can be performed under local anesthesia with or without sedation or under general anesthesia. It can be performed as an isolated procedure or in the setting of GRA/SRS reassignment surgery. Simply speaking, the incision is made along the median raphe or midline of the scrotum. The testicles and spermatic cord are isolated and the cord is clamped and tied at the inguinal ring. The incision on the scrotum is closed with dissolving sutures. No skin is removed. This is important for those considering a GRS/SRS procedure in the future. This skin can be used during GRS/SRS for lining the new vaginal canal.
Orchiectomy Candidates
Ideal candidates are generally healthy and have met the following criteria according the WPATH standards of care.
- Two letters of referrals (one from a MHP – psychotherapist who follows the patient and one second opinion letter from a MHP that has evaluated the patient)
- Persistent, well documented gender dysphoria
- Capacity to make a fully informed decision and to consent for treatment
- Age of majority in a given country
- If significant medical or mental health concerns are present, they must be well controlled
- 12 continuous months of hormone therapy as appropriate to the patient’s gender goals (unless the patient has a medical contraindication or is otherwise unable or unwilling to take hormones).